Institutional Racism in Prostate Cancer Screening Among Black Men
The BioSpy story started when a white American asked a black Jamaican doctor one question: "What would you use as the cut-off for a healthy PSA level in a 45 year old person of African descent who presented for prostate cancer screening?"
The surgeon quickly recalled his training and regurgitated the information. Thirty minutes later, after reviewing six of the seven peer-reviewed journal articles cited in this article, he said, "Doctors aren't being taught this. This whole time we've been using ratio's and cut-off levels designed for a 55 year old white man. Something has to be done."
The doctor was not alone. In fact, physicians have been calling for completely separate screening guidelines for black men, recognizing different cut-off levels, different approaches and screening at an earlier age.¹
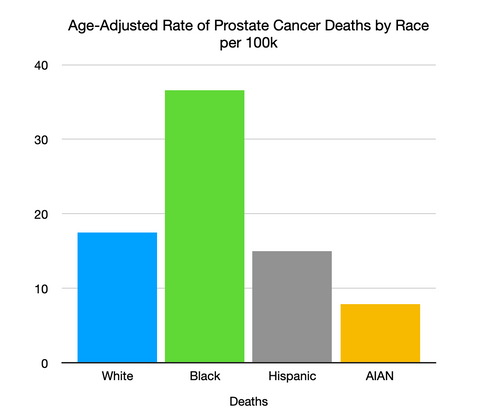
If you're reading this article, you probably already know that prostate cancer affects men of African decent at a disproportionately higher rate than their white peers. While the reasons are many, the outcomes are the same: Black men do not live as long as white men², and do not visit the doctor as often as white men.³
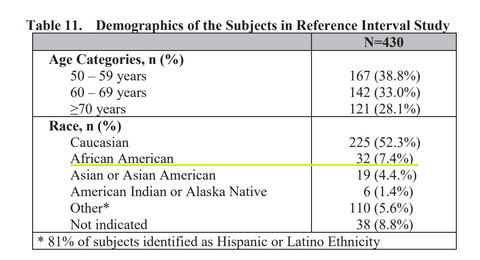
Not withstanding the above, the US Preventative Services Task Force (in 2012) recommended to not screen for prostate cancer, as harms could outweigh the benefits. Not surprisingly, screening rates declined a further 10% in persons of African decent, a population genetically predisposed to more frequent and more aggressive prostate cancer, and 2.2x more likely to die from prostate cancer. To further exacerbate the problem, new prostate cancer screening tests were developed after the US Preventative Services Task Force much-maligned opinion, by US companies, and approved by FDA, using populations that underrepresent African Americans by nearly 50% (See screen capture from FDA approval order below on this test's study demographics).⁴
The development of the test, and its subsequent approval, came with the knowledge that black men were 5x more likely to have prostate cancer in their lifetime, and 2.2x more likely to die from prostate cancer.⁵ The medical community is also acutely aware that Black men have higher PSA levels than their white counterparts, and are much less likely to be screened for prostate cancer.⁶
Further investigation reveals that African Americans, when compared with whites, had lower odds of receiving a Pap test, rectal exam, smoking cessation counseling, or even mental health advice.⁷
The takeaway was obvious: Help was not on the way. Racial disparities (and overt racism with respect to quality of care, research and development, and clinical trials) in health care are very real, and very deadly.
18 months later, BioSpy Prostate IQ™ was born. A test that does not require a blood draw, is stratified by race and age, and an additional baseline free PSA analyte was added (known to reduce the number of unnecessary biopsies by 25-40%). We learned a valuable lesson from the 2012 Joint Taskforce Guidelines: Ignoring know problems is not a solution. Telling black men to be a "prisoner of hope" is not a solution. Screening and early detection for prostate cancer (like all cancers) is key, and institutional racism is alive and well...for now.
SOURCES:
1. Shenoy D, Packianathan S, Chen AM, Vijayakumar S. Do African-American men need separate prostate cancer screening guidelines? BMC Urol. 2016 May 10;16(1):19. doi: 10.1186/s12894-016-0137-7. PMID: 27165293; PMCID: PMC4862049.
2., 3. Hill, Ndugga, Artiga, Key Data on Health and Healthcare by Race and Ethnicitiy. KFF Health Policy and Resources 2023 Mar. https://www.kff.org/racial-equity-and-health-policy/report/key-data-on-health-and-health-care-by-race-and-ethnicity/
4. US Food and Drug Administration Pre Market Notification Number P170037: Sangia Total PSA Test. 2019 Jan https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpma/pma.cfm?ID=414765
5. Shungu N, Diaz VA, Perkins S, Kulshreshtha A. Physician Attitudes and Self-reported Practices Toward Prostate Cancer Screening in Black and White Men. Fam Med. 2022;54(1):30-37. https://doi.org/10.22454/FamMed.2022.474827.
6. Franks P, Fiscella K, Meldrum S. Racial disparities in the content of primary care office visits. J Gen Intern Med. 2005 Jul;20(7):599-603. doi: 10.1111/j.1525-1497.2005.0109.x. PMID: 16050853; PMCID: PMC1490148.
7. Lillard JW Jr, Moses KA, Mahal BA, George DJ. Racial disparities in Black men with prostate cancer: A literature review. Cancer. 2022 Nov 1;128(21):3787-3795. doi: 10.1002/cncr.34433. Epub 2022 Sep 6. PMID: 36066378; PMCID: PMC9826514.



